QUOTE(roystevenung @ Mar 2 2019, 08:10 AM)
If you haven't noticed, I am trying to help you resolve this issue. It would be better to find solution to the problem rather than hyping on it, don't you agree?
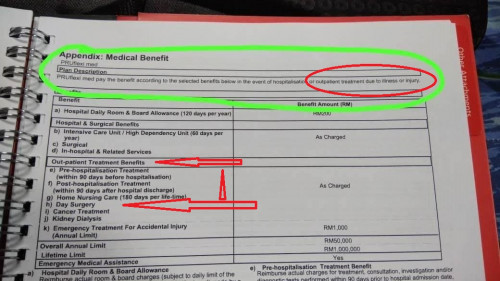
I am not diverting the main issue and I am still saying that Day Surgery is covered in PruFlexi Med as mentioned in the policy book and it is even mentioned in the brochure. For your information, any official letter by Prudential can only be issued by HQ, therefore if you insist on it, you need to take that to HQ.
Point is, if you go see the Dr and he admit you with Guarantee Letter (GL) -> normal hospitalization with GL admission is required if the case is cover able by checking the Exclusions.
However, if it is a non-emergency cases and can be done as a Day Surgery, the Dr will still need to apply for the Guarantee Letter 7 days prior to the day surgery. Between the date of the surgery, Prudential will also check whether the case is cover able based on the Exclusions of the policy, pre-existing, hereditary, congenital etc.
If the GL is declined for whatever reasons, any further treatment is on your own. In this case you may escalate this issue to the Bureau as stated in your third page of the policy if you want to dispute on the claim.
The Dr need to request for a GL, otherwise if you were to seek treatment before getting the GL, it is still a grey area whether the case is cover able.
This is why agent's always advice client to go to panel hospitals (to avoid the pay and claim process) as some illness are not cover able after checking the Exclusion. It's better to get the GL to know for sure that the case is cover able.
Thanks for the help, Yes,im getting the GL to confirm Prudential will reject or approve but they gave nothing until now. Next week we shall see. Its for full admission so i dont see an issues on that. IF THEY DIDNT REJECT MY OUTPATIENT TREATMENT/DAY SURGERY , i wont be posting here!I am not diverting the main issue and I am still saying that Day Surgery is covered in PruFlexi Med as mentioned in the policy book and it is even mentioned in the brochure. For your information, any official letter by Prudential can only be issued by HQ, therefore if you insist on it, you need to take that to HQ.
Point is, if you go see the Dr and he admit you with Guarantee Letter (GL) -> normal hospitalization with GL admission is required if the case is cover able by checking the Exclusions.
However, if it is a non-emergency cases and can be done as a Day Surgery, the Dr will still need to apply for the Guarantee Letter 7 days prior to the day surgery. Between the date of the surgery, Prudential will also check whether the case is cover able based on the Exclusions of the policy, pre-existing, hereditary, congenital etc.
If the GL is declined for whatever reasons, any further treatment is on your own. In this case you may escalate this issue to the Bureau as stated in your third page of the policy if you want to dispute on the claim.
The Dr need to request for a GL, otherwise if you were to seek treatment before getting the GL, it is still a grey area whether the case is cover able.
This is why agent's always advice client to go to panel hospitals (to avoid the pay and claim process) as some illness are not cover able after checking the Exclusion. It's better to get the GL to know for sure that the case is cover able.
IM NOT HYPING, IM getting PUBLIC HELP/INFORM THEM TO CONFIRM OUTPATIENT TREATMENT for this PLUflexi MED Card is Cover or not, its so simple.. IF YOU CANT CONFIRM IT WITH BLACK AND WHITE, Its just TALKING only.. whats different with AGENT THAT SAY ALMOST EVERYTHING IS COVER WHEN We are BUYING IT. Dont FOOL US please. POLICY BOOK Stated clear its COVER and now emergency calling HOTLINE and AGENT SAY ITS NOT COVER. PAY YOURSELF FIRST
This post has been edited by max880930: Mar 2 2019, 03:18 PM


 Mar 2 2019, 03:06 PM
Mar 2 2019, 03:06 PM

 Quote
Quote

 0.0251sec
0.0251sec
 0.87
0.87
 5 queries
5 queries
 GZIP Disabled
GZIP Disabled