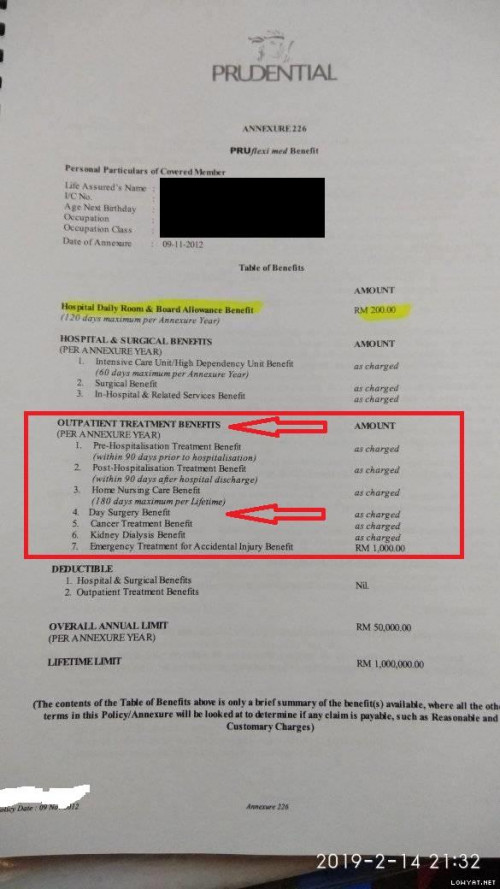
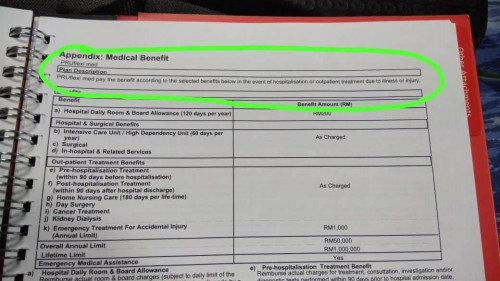
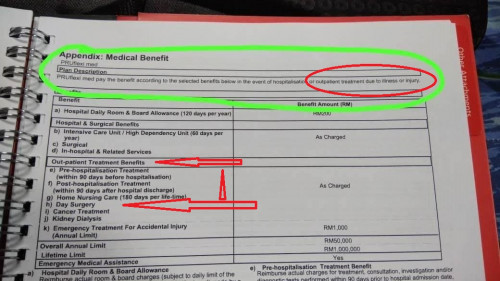
I can confirm to you that Day Surgery benefit is applicable to ALL Prudential medical card (irrespective of old or new). As mentioned earlier, the reason for the insurer to have the Day Surgery Benefit is to cut the cost of having minor admission.
I believe the Customer Service has misunderstood on your request and for that I do apologise as they are not directly involved in the claims process. There are a lot of things not made known to the Customer Service especially when it comes to claims

For example the cataract surgery, before the introduction of the Day Surgery Benefit, the client will still need to be admitted for 1 day even though it is not required. This incur room charges of 1 day, which translates to extra cost to the insurer.
For your information, the Day Surgery Benefit is a PRE-PLANNED, non emergency day surgical procedure with the ISSUANCE of Guarantee Letter.
This has to be applied 7 days before the intended surgery. The benefit of this is that the client do not need to wait for the issuance of the Guarantee Letter. This means that it has to be requested by a Panel Hospital, but unfortunately in your case, PPUM is not under a panel hospital.
Since you had been admitted to the PPUM, for the PPUM claims, my advice is to get the Dr to write the Doctor’s Report as stated in my previous reply.
I believe the confusion is due to Customer Service and how Day Surgery works. In your case for PPUM, you should claim under normal admission, not under day surgery.
May I concur that you were not informed by your agent that if you were admitted to a non-panel hospital, you need to pay and file a claim later? If that is the case, at least you may feed back to your agent for his/her improvement.
Yes it is a known fact that if you are admitted to a non-panel, it is on reimbursemnent basis aka, PAY AND CLAIM, irrespective of ANY INSURER.
If you are overseas on a holiday, unless it is accidental, you will also need to pay and claim and the reimbursement will be customary to what is being charged in a hospital in Malaysia. For eg, dengue at Singapore, cost SGD 8K, of which you will only be reimbursed RM10K.
There are many reasons why some hospitals are not a panel for the insurer as there are lots of criteria to qualify to be a panel. The Medical Insurance is a MULTI-MILLION ringgit business and for us to qualify the hospital, it has to be of certain standards, from the equipments, specialist, facilities, billings, comformance of standards and many more.
The medical reports/test & billing details must be made available to the insurer when a person is admitted to the hospital. Some of the doctor reports can only be given after 2 months, in
which directly translates to delay in paying the claims to the customer.FYI the PruFlexi Med will reimburse the room differences back to the customer, eg, if your room is RM200, and you stayed in a RM150 room, Prudential will reimburse RM50/day once you are discharged from the panel hospital. The fastest reimbursement that I had seen is 5 working days upon discharge. Of course all these are with facts and proof, not simply bla at an open forum
See above on the process for getting treatment at a non-panel hospital.
You are right to the Point. PRUDENTIAL CUSTOMER SERVICE IS NOT PROFESSIONAL OR should i say what they say cannot be trusted which MISLEAD US that Day surgery, Outpatient treatment is not cover AND THEY WAN US TO PAY FIRST And Claim later
i called at least 3 times and they saying the same thing everyone of them. Its doesnt matter its government hospital or private, ITS NOT COVER! SO DO NOT DO Day surgery or outpatient treatment.
I had admitted to PPUM and upon confirmation ON outpatient treatment is NOT COVER i Immediately TRANSFER OUT to PANEL HOSPITAL SUNWAY. and upon arrival there, prudential say the bloodly hell same thing that outpatient treatment is NOT COVER and yes i WILL do FULL Admission and GONNA STAY TWO WEEKS IN PRIVATE HOSPITAL by Spending PRUDENTIAL CUSTOMER MONEY SINCE PRUDENTIAL REJECTED MY OUTPATIENT TREATMENT
UNTIL NOW, IM PAYING MY OWN MONEY FOR THE ADMISSION/DOCTOR VISIT and WAITING TO SEE WHAT DRAMA THIS PRUDENTIAL WILL DO upon my discharge.
IF Customer Service cannot be trusted on what they say and AGENT say its NO COVER also and this PRUflexi med cannot be used for day surgery/outpatient treatment in the END STILL WE ARE THE ONE THAT PAYING IT. Im doing Pre-admission for full surgery instead of DAY SURGERY now since they rejected it.
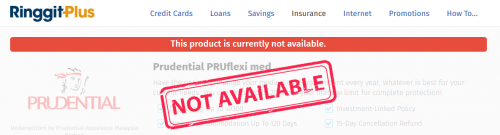
How many people have prudential FOOLED? i heard prudential is not paying hospital thats why they are not listed/banned as panel. Prudential even put some ambassador at certain private hospital BUT THEY CONFIRMED ME That OLD PLAN PRUflexi med IS NOT COVER HAHA.. and here someone agent still telling me that its cover..
Maybe you can show me which day surgery listing that mention PRUflexi med cover... the new plan have it, old plan dont have. The link you give is only applicable for new plan even they dont mention which plan have it. PRudential AMBASSADOR at hospital do pass me that and mention its for new plan only. Maybe a PRUDENTIAL letter with title head will be sufficient. I Requested for that letter before and refused also.


 Feb 28 2019, 12:29 AM, updated 7y ago
Feb 28 2019, 12:29 AM, updated 7y ago
 Quote
Quote




 0.0237sec
0.0237sec
 1.06
1.06
 6 queries
6 queries
 GZIP Disabled
GZIP Disabled