QUOTE(max880930 @ Feb 28 2019, 12:29 AM)
Dear All old Prudential plan owner!! Beware!
im surprise when i admitting for government hospital (PPUM) for day surgery (RAI 131) .Prudential customer line: 03-2116 0228
Upon checking my insurance policy, She CONFIRMED with me that OUTPATIENT TREATMENT/DAY SURGERY is not COVERED/CLAIMABLE unless Accident by my cashless insurance card.
Let me try to help you resolve this issue. im surprise when i admitting for government hospital (PPUM) for day surgery (RAI 131) .Prudential customer line: 03-2116 0228
Upon checking my insurance policy, She CONFIRMED with me that OUTPATIENT TREATMENT/DAY SURGERY is not COVERED/CLAIMABLE unless Accident by my cashless insurance card.
If you had been admitted to the PPUM (not as Day Surgery since there isn't any surgery being performed), you can submit the following for claims consideration:-
1. The original PPUM Bills & any tests/reports done
2. The Claim Form (Doc ID 11601067)
3. The Doctor's Statement (DocID 11601007) - to be filled up by the PPUM Dr that treated you
Item 2 & 3 can be obtained from your agent or Prudential website. Before submitting the claim, please make a scan copy for future references.
Item 3 is required because PPUM is not a panel hospital for Prudential, therefore a GL is unable to be issued.
QUOTE
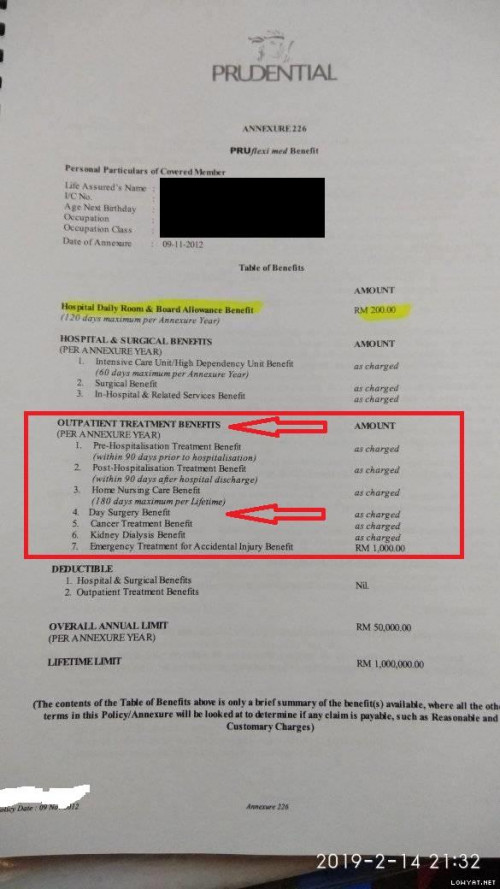
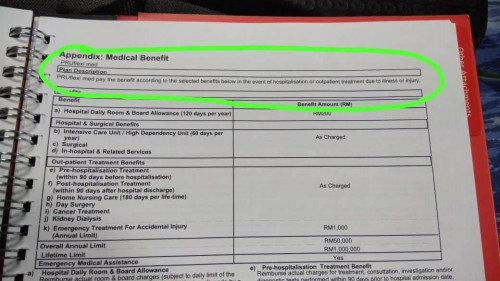
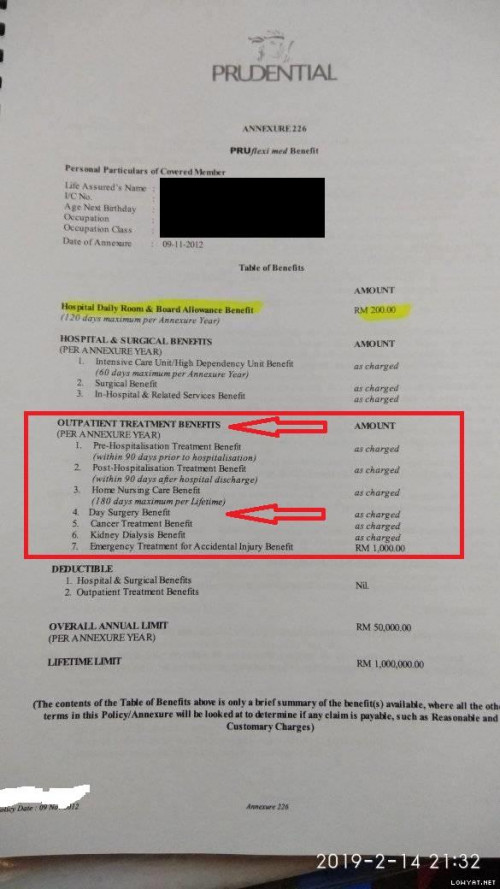
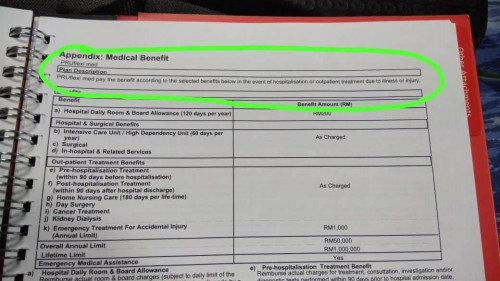
PRUflexi MED since 2012. 7 Years old medical card!
Upon my questioning on agent, they say only NEW plan cover day surgery and outpatient treatment. You will need to go private hospital and try to do full admission.
I Checked back my policy book and it written clearly OUTPATIENT TREATMENT is cover. Currently im paying all the Private hospital bill myself up to 2k+ so far and lucky hospital didnt take alot deposit since they know im disputing with insurance now. Until NOW im not sure its Claimable OR NOT.
Whether it is an old or new medical card, it does cover DAY SURGERY. However, it is required for a surgery to be performed and in your case there isn't any surgery. Therefore it is not claimable under day surgery. Since there is an admission to PPUM, you may proceed to submit the claim as mentioned above.Upon my questioning on agent, they say only NEW plan cover day surgery and outpatient treatment. You will need to go private hospital and try to do full admission.
I Checked back my policy book and it written clearly OUTPATIENT TREATMENT is cover. Currently im paying all the Private hospital bill myself up to 2k+ so far and lucky hospital didnt take alot deposit since they know im disputing with insurance now. Until NOW im not sure its Claimable OR NOT.
A list of Day surgery procedure can be downloaded <<Here>>
The "Day Surgery" was introduced as it DRASTICALLY REDUCES the medical claim BILL as most cases there is no need to be admitted to hospital, eg, Cataract Surgery.
QUOTE
<a href='https://www.prudential.com.my/en/our-services/make-a-claim/day-surgery-benefits/' target='_blank'>https://www.prudential.com.my/en/our-servic...rgery-benefits/ 
So this is the scenario that will happen in future.. you got sudden stroke or chest pain or faint and send by ambulance to hospital government or private..after done some minor surgery, medicine and you can back home the same day or you choose for for so call outpatient /day surgery..
YOUR OLD PRUDENTIAL MEDICAL CARD WONT BE ABLE TO CLAIM IT/ ADMISSION with the card and its not COVERED cause its NOT ACCIDENT
PRUFLEXI MED plan. please double check with your agent or simply call to the customer line. AGENT will Mentioned New plan is covered and who didnt update it... eat yourself..
ExampleSo this is the scenario that will happen in future.. you got sudden stroke or chest pain or faint and send by ambulance to hospital government or private..after done some minor surgery, medicine and you can back home the same day or you choose for for so call outpatient /day surgery..
YOUR OLD PRUDENTIAL MEDICAL CARD WONT BE ABLE TO CLAIM IT/ ADMISSION with the card and its not COVERED cause its NOT ACCIDENT
PRUFLEXI MED plan. please double check with your agent or simply call to the customer line. AGENT will Mentioned New plan is covered and who didnt update it... eat yourself..
1. If a person go see the Dr and the Dr prescribe High Blood Pressure pill, there wasn't any admission, the cost have to be paid by yourself. However, do keep the bill. It can be claimable if there is admission (for the PruFlexi Med the Pre Hospitalization is 90 days) later. Pre & Post Hospitalization IS OUTPATIENT TREATMENT.
2. However, if a person have breathing complication/extreme nausea/fainting, admitted and does angiogram, then it is covered. Any medication given by the Dr that addresses to the problem, will be covered. If the Dr prescribe you Vitamin, naturally, it will not be covered.
3. Once discharge there is another 90 days of Post Hospitalization (which is to be done as OUTPATIENT), pay and claim.
Ps. I also have client who has hyperthyroid, initial RAI meds (which is not covered) and after a month, opted for surgery as it was getting bigger and painful. Surgery done was covered together with the earlier pre-hospitalization.
This post has been edited by roystevenung: Feb 28 2019, 11:25 AM


 Feb 28 2019, 11:11 AM
Feb 28 2019, 11:11 AM

 Quote
Quote



 0.2028sec
0.2028sec
 1.48
1.48
 6 queries
6 queries
 GZIP Disabled
GZIP Disabled