QUOTE(lifebalance @ Aug 20 2019, 11:49 AM)
I'm still quite surprised that you did all the test above during hospitalization and they mention its not covered under the GL?

probably can you show us a copy of the Allianz policy on what is covered during hospitalization ?
1) Went to specialist with referral letter from clinic, ask to do scope
2) Admitted around 9:30AM, my operation (endoscropy) is scheduled at 1PM
3) Nurse asked if I want to do blood test/ultrasound first even though my insurance haven't give approval yet
4) Checked with agent, he said once admitted, blood test/ultrasound are covered - so I proceed
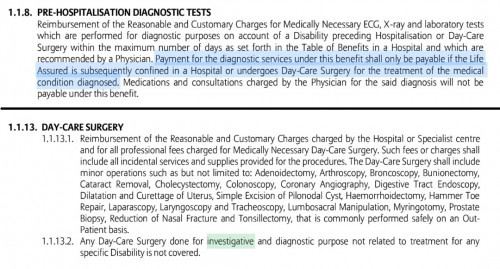
5) Around 12PM, staff told me insurance only give "Non Guarantee" status and that I have to pay myself first. So I contacted my agent and he checked with Allianz. Apparently scope is considered "investigative nature", I can only claim if I'm getting surgery later. I also won't be able to claim if there's nothing found during the procedure.
6) The staff did ask if I still want to proceed, which I did because I was already changed into hospital gown and already came this far (been suffering since May, just want to get it over with).
So yes in a way the agent did inform me that it's not claimable if no surgery, but I still think it's a bit too late.
Then again, gastric problems are most likely healed thru meds/probiotics so anyhow I won't get to claim too even if something was found during the scope, since no surgeries will be involved?
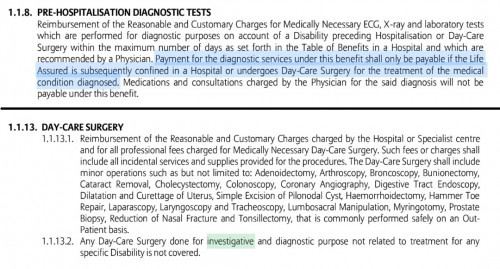
I attach screenshot from the policy what I think is related to my case


 Aug 19 2019, 05:31 PM
Aug 19 2019, 05:31 PM
 Quote
Quote
 0.0906sec
0.0906sec
 1.14
1.14
 7 queries
7 queries
 GZIP Disabled
GZIP Disabled